Overview and Statistics
Antipsychotics are prescription medications developed to treat mental disorders such as schizophrenia, paranoia, hallucinations, and the mania associated with bipolar disorder. They are also known as “major tranquilizers” because they calm and suppress certain mood-controlling chemicals in the brain, such as dopamine.
Antipsychotics have been in use since the 1950s, and for years were used to treat elderly people with dementia. In 2005, however, after extensive research, the Food and Drug Administration (FDA) issued a black-box warning on antipsychotics, advising that people with dementia who took the medications were at increased risk of heart failure, stroke, infection, and death.
Unfortunately, antipsychotics are widely used in nursing homes to address patients that caregivers find difficult, even though federal law prohibits the use of antipsychotics as “chemical restraints imposed for purposes of discipline or convenience, and not required to treat the resident's medical symptoms.” Nursing homes should not administer antipsychotics without a documented medical need or as a substitute for good, individualized care. High quality and well-staffed nursing homes prescribe antipsychotics at a much lower rate.
Statistics on this issue are alarming. According to research being done at the University of California, San Francisco, as many as 1 in 5 nursing home residents are given unnecessary and dangerous antipsychotics. Other sources have estimated that 26% of nursing home residents in general are given antipsychotics, while dementia patients are given the prescription drug 40% of the time.
Further Dangers of Antipsychotics
Besides the increased risk of a serious health condition and/or sudden death, there are other side effects of antipsychotics that can alter your loved one’s interaction with the world. The National Consumer Voice, a nursing home resident advocacy group, describes the common effects of these particular drugs thus:
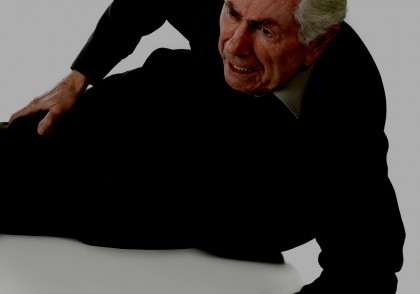
“Antipsychotics can be so powerful that they sedate residents to the point where they become listless and unresponsive. Residents may be slumped in wheelchairs or unable to get up from bed; they may no longer be able to participate in activities they enjoy or even talk with their loved ones.”
Besides a general sedation, anxiety, and the depression of motor, cognitive, and perceptual function, the administration of antipsychotics significantly increases the risk of falls in elderly patients, which is already the number one cause of injury in adults over 65. Since antipsychotics can also weaken bones and contribute to osteoporosis in older adults, the risk of fracture is compounded by the drug. Multiple studies have confirmed this pattern, including research which shows that people given antipsychotics “on a scheduled basis had a nearly threefold increase in falls.” In fact, several types of drugs are associated increased risk of fall, including antidepressants, hypnosedatives, and benzodiazepines.
Taking Action
If nursing homes are prescribing and/or administering antipsychotics to a loved one without a doctor’s order, medical necessity, and the patient’s informed consent, they are in violation of federal law. In addition to compensation for medical conditions that stem from the use of antipsychotics, you and/or your loved one may file a lawsuit claiming damage for the emotional pain and suffering associated with the medication’s effect. To explore your options for litigation, contact the law firm of Dalli & Marino today. You can call our offices anytime at 888-465-8790, or fill out our online form for a free case evaluation.
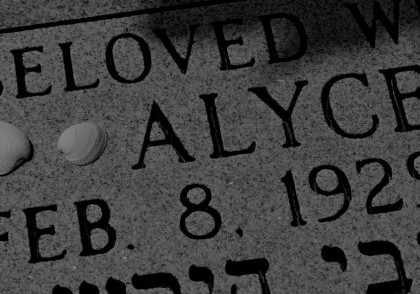
Case Study – [MC]
“But for that dosing error… Mom would still be with us.” DATELINE…
Case Study: Wrongful Death
Nursing Home Abuse: Case Study 19: Wrongful Death in a Nursing Home
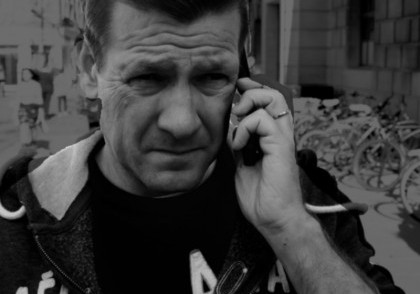
Case Study: Nursing Home Abuse — From a Distance
You can’t be there every minute. But what of the warning signs for nursing home abuse?
Cases of Nursing Home Abuse
Review our portfolio of case studies covering numerous aspects of nursing home abuse: falls, bedsores, over-medication, neglect.
Case Study: Where is Everyone?
Nursing Home Abuse Case Study: Understaffing or neglect in a nursing home can cause severe loneliness, depression, loss of appetite or ignore health warning signs.
Case Study: Nursing Home Falls
Nursing Home Abuse: Despite best practices intended to reduce the incidence of falls, they remain a common cause for nursing home injuries.
Case Study: It Starts with Bruising
Nursing Home Abuse: Bedsores caused by neglect
Case Study: Nursing Home Bedsore
Nursing Home Abuse: Bedsores can lead to fatal complications, including organ failure and even cancer.
Case Study: I Never See A Doctor When I Request One
Nursing Home Abuse Case Study: Patients fail to receive prompt attention from nursing home physicians.
Case Study: Medication Error
Nursing Home Abuse Case Study: A medication error leads to dangerous health complications or death.