Why do so many medication errors occur?
When you hear concerning data about the possibility of a loved one receiving incorrect medication, it is natural to wonder why. Below is a list of possible causes of medication errors in nursing homes:
- Basic Human Error
- Transcription Error
- Frequent Distractions/Care Changes
- Poor Communication
- Pharmacy Dispensing
- Medication Unavailable
- Medication Name Confusion
- Following Policies & Procedures
- Too Much Workload/Overtime
- Shift Change
- Product Labeling
- Pharmacy Delivered Wrong Medication
- Packaging Design
- Inadequate Information
- Improper Training
- Illegible Handwriting
- Short staffng
- Inadequately trained medical staff
Who is to blame?
The medication your loved one receives most likely passes through many hands before it reaches them. There are many parties that may be liable for errors. If the nursing home does not have clearly stated procedures and comprehensive training for all their employees, they may be responsible for the error, in addition to the nurse or caretaker who administered the medication. The physician who prescribes the drug may be negligent if they fail to consider potential negative drug interactions. In some cases, pharmacists who make mistakes in measuring and distributing the medication may also be found negligent.
Do I have access to my loved one’s medical records?
It is often a good idea to request copies of medical records when concerned with the treatment of a parent or other elderly relative. A resident and their representative have a right to view and receive copies of medical records. Authorized representatives of a resident will usually be established upon the resident’s entry into the nursing home, and each nursing home will have their own procedures and forms used to authorize representation.
Federal regulation Section 483.10 lays out basic rights of long term care facility residents. These include the following rights of a resident and their representative:
(i) Upon an oral or written request, to access all records pertaining to himself or herself including current clinical records within 24 hours (excluding weekends and holidays); and
(ii) After receipt of his or her records for inspection, to purchase at a cost not to exceed the community standard photocopies of the records or any portions of them upon request and 2 working days advance notice to the facility.
Does the nursing home have to alert me before they change my loved one’s medication?
Yes, nursing homes should alert you when there are any changes to your relative’s condition, if you are their legal representative. In fact, nursing homes are legally obligated to alert the resident, a physician, and the legal representative or other family member for a variety of reasons including
- any accident involving the resident causing injury which might require medical attention
- significant changes in the resident’s physical, mental, or psychosocial state
- the need to alter treatment significantly; i.e. add or discontinue treatments
- the decision to transfer the resident to another facility
In addition, the nursing home should alert you if they decide to change your loved one’s room or roommate and if any of the laws governing their legal rights are altered.
If I suspect that they are mismanaging my relative’s medication, who should I talk to?
There are many people you can approach about the problem, depending on the situation. If you trust your loved one's physician or the nursing home supervisor, you can talk to them about the employees who manage your relative's medication on a daily basis. If your relative is cognizant and aware, they may be able to give you information. Alternatively, you may file a complaint through the grievance system in place at any Medicare/Medicaid-certified nursing home or contact one of the many government agencies in place to protect elder home abuse victims such as Adult Protective Services who will assign a case manager. You may also call 911.
Since medication errors are not always considered abuse because they may not be intentional, it is advisable to speak with legal counsel to determine the best course of action. Our firm has worked extensively on such cases and can help support you through the investigation and litigation process. Contact the law firm of Dalli & Marino today for a free case evaluation.
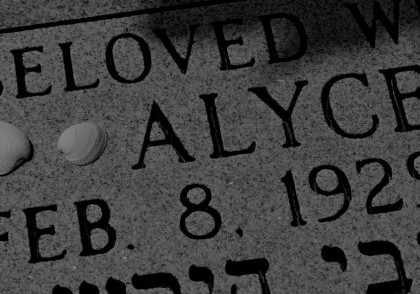
Case Study – [MC]
“But for that dosing error… Mom would still be with us.” DATELINE…
Case Study: Wrongful Death
Nursing Home Abuse: Case Study 19: Wrongful Death in a Nursing Home
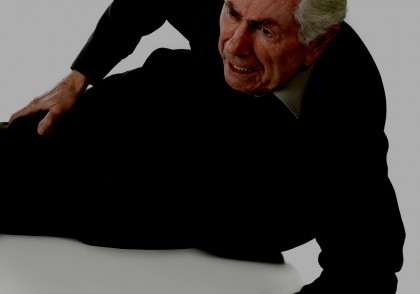
Case Study: Nursing Home Abuse — From a Distance
You can’t be there every minute. But what of the warning signs for nursing home abuse?
Cases of Nursing Home Abuse
Review our portfolio of case studies covering numerous aspects of nursing home abuse: falls, bedsores, over-medication, neglect.
Case Study: Where is Everyone?
Nursing Home Abuse Case Study: Understaffing or neglect in a nursing home can cause severe loneliness, depression, loss of appetite or ignore health warning signs.
Case Study: Nursing Home Falls
Nursing Home Abuse: Despite best practices intended to reduce the incidence of falls, they remain a common cause for nursing home injuries.
Case Study: It Starts with Bruising
Nursing Home Abuse: Bedsores caused by neglect
Case Study: Nursing Home Bedsore
Nursing Home Abuse: Bedsores can lead to fatal complications, including organ failure and even cancer.
Case Study: I Never See A Doctor When I Request One
Nursing Home Abuse Case Study: Patients fail to receive prompt attention from nursing home physicians.
Case Study: Medication Error
Nursing Home Abuse Case Study: A medication error leads to dangerous health complications or death.